OUR MINIMALLY INVASIVE SURGEONS ARE FIRST ON LONG ISLAND APPROVED TO IMPLANT MAGNETIC BAND TO PREVENT HEARTBURN
New LINX Procedure Represents Latest Advance for Treating Acid Reflux

are performing the new LINX procedure to treat GERD.
STONY BROOK, NY, November 6, 2013 — The Department of Surgery's General Surgery Division is now performing an innovative new procedure to implant a small magnetic band to help prevent gastric reflux in patients who suffer from gastroesophageal reflux disease (GERD), commonly known as heartburn, or acid indigestion, the most common symptom of GERD.
Our surgeons are the first on Long Island to be specially trained and certified to use the LINX® Reflux Management System. Use of this innovative system further demonstrates our department's commitment to using leading-edge technology to lead the way in patient care.
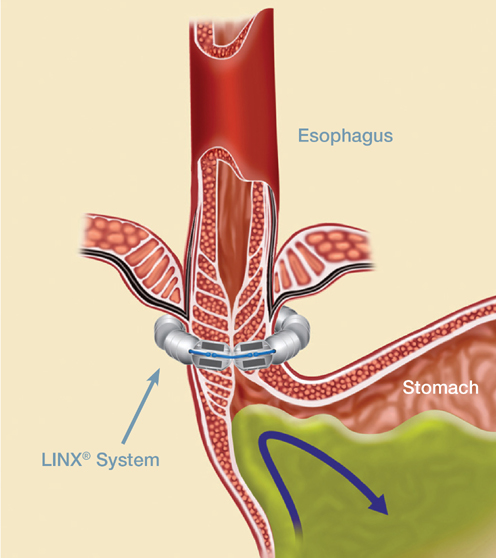
The new minimally invasive surgical procedure represents the latest advancement in the treatment of GERD. Surgeons implant the LINX band — a small, flexible band of titanium beads with magnetic cores — around the patient's esophagus just above the stomach. The magnetic attraction between the beads strengthens the weakened esophageal sphincter's barrier function. The procedure usually takes less than an hour to perform.
The band is strong enough to allow food and liquids to pass normally to the stomach, but immediately closes after swallowing to restore the magnetic barrier to reflux. Following the procedure, patients are able to resume a normal diet, and will typically resume normal activities in less than a week.
Studies have shown the banding procedure decreases esophageal acid exposure, improves reflux symptoms and quality of life, and allows cessation of proton pump inhibitor medication in most patients.
"This new procedure represents a substantial advancement in our ability to treat patients who suffer from GERD," says Mark A. Talamini, MD, professor and chairman of surgery, and founding director of the Stony Brook Medical Innovation Institute.
Dr. Talamini, who performs the LINX procedure, adds: "In addition to excellent clinical results, LINX provides many lifestyle benefits compared to the traditional surgery for reflux called Nissen fundoplication. Studies show that implanting the magnetic band often reduces or eliminates the need for medications, and offers improved quality of life for our patients."
Also performing the procedure here are fellow general surgeons Aurora D. Pryor, MD, professor of surgery, chief of general surgery, and director of the Stony Brook Bariatric and Metabolic Weight Loss Center; and Dana A. Telem, MD, assistant professor of surgery and associate director of the Bariatric and Metabolic Weight Loss Center.
Drs. Talamini, Pryor, and Telem all have advanced laparoscopic skills, and are leaders in the area of minimally invasive surgery. The LINX band is implanted laparoscopically.
"The LINX procedure, which uses the novel LINX technology, is indicated for patients diagnosed with reflux who continue to have chronic reflux symptoms despite maximum medical therapy," says Dr. Pryor.
"GERD is a caused by a mechanical defect and requires a mechanical solution, which is achieved through the minimally invasive LINX procedure," Dr. Telem says. "As the first surgeons on Long Island approved to perform this procedure, we will be able to directly benefit many patients who suffer from acid reflux."
Over 30 million Americans suffer from acid reflux each month. The symptoms of GERD include heartburn, regurgitation, sore throat, cough, and chest pain. When left untreated, reflux disease can lead to serious complications, such as esophagitis, stricture, Barrett's esophagus, and esophageal cancer.
The LINX device was FDA approved in March 2012 after ten years of development and testing, including two clinical trials with 144 patients. A total of 400 implant procedures were performed over five years of clinical use. In one trial, 90% of patients achieved a reduction in time exposed to acid, with 93% reporting a 50% or greater reduction in GERD over two years. Ninety-two percent of patients were off daily proton pump inhibitors (PPIs), a group of drugs whose main action is a pronounced and long-lasting reduction of gastric acid production, after two years. The number of patients reporting regurgitation dropped dramatically from 57 to 1.
| Several studies demonstrate the effectiveness and safety of the LINX procedure. Recently, two major studies were published in the New England Journal of Medicine (NEJM) and the Journal of the American College of Surgeons (JACS). In February 2013, the NEJM published a study involving 14 U.S. and European medical centers which found that a majority of patients were able to substantially reduce or resolve their reflux symptoms after the LINX band was implanted, while eliminating use of their reflux medications. Severe regurgitation was eliminated in 100% of patients, and 93% reported a significant decrease in the need for medication. More than 94% of patients reported satisfaction with their overall condition after having the LINX system, compared to 13% before treatment while taking medication. In July 2013, JACS reported on a six-year study of 100 patients with GERD who had been on daily reflux medications for several years before undergoing laparoscopic surgery to have the LINX system implanted. Three years after the band was implanted, 93% of patients reported significant improvement in their quality of life, and 85% reported complete cessation of their acid reflux medication. There were no intraoperative complications. |
For consultations/appointments with our surgeons who provide LINX, please call 631-444-2274. Watch this video (1:24 min) to see how the LINX band works: