Mediastinal tumors are benign or cancerous growths that form in the mediastinum; that is, the area in the middle of the chest between the sternum (breastbone) and spinal column.
The mediastinum, which separates the lungs, houses the heart, esophagus, trachea, great vessels, thymus, and lymph nodes.
Mediastinal tumors are relatively uncommon. They tend to be more common in young and middle-aged adults, but they may affect people of all ages.
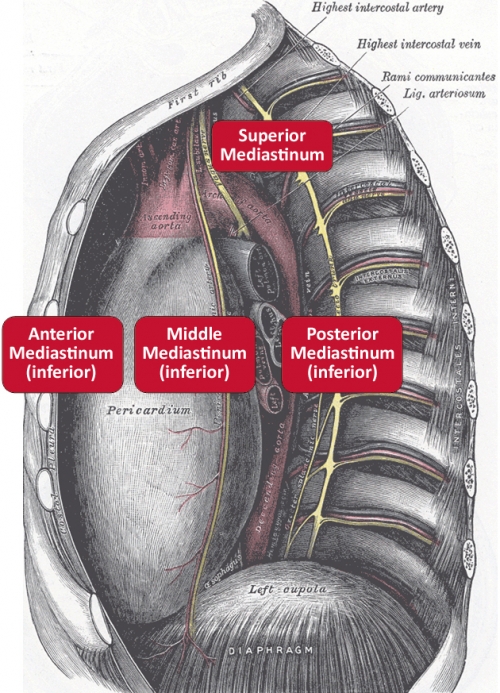
These tumors develop in one of three areas of the mediastinum: the anterior (front), the middle, or the posterior (back). Different tumors are more common in certain age groups.
Children usually develop tumors in the back of the mediastinum, and they are often benign tumors. Adults usually develop them in the front, and these tumors can be cancerous.
Mediastinal tumors often pose a diagnostic and therapeutic challenge to thoracic surgeons. Surgical skill and experience, thus, are critical to successful treatment outcomes.
Here, Henry J. Tannous, MD, a leader on our thoracic surgery service and specialist in mediastinal tumors, answers frequently asked questions about these tumors and their management.
Q: What causes mediastinal tumors to form?
A: Depending on etiology, a mediastinal tumor can be caused by an enlarged lymph node, or a gland such as the thymus, thyroid, or parathyroid. It can also be caused by a cyst originating from the pericardium (the sac that houses the heart), the bronchus, or the esophagus. Another cause of a mediastinal tumor can be a cancer that has spread into the mediastinum.
Q: How many different kinds of mediastinal tumors are there?
A: Mediastinal tumors can be classified by location (anterior, middle, and posterior) or by benign versus malignant. An anterior mass is the most common, and it could represent a thymoma, a lymphoma, a germ cell tumor, or a thyroid mass.
Q: What are the common mediastinal tumors?
A: Thymomas are the most common mediastinal tumors. They start in the thymus, which is a small organ in the front part of the chest under the breastbone. They represent one third of anterior mediastinal tumors and 15-20% of all tumors.
Thymomas could be associated with myasthenia gravis, which is a disease of the neuromuscular junctions causing weakness, and which is present in about half of all patients with thymoma at some stage.
Thymomas grow slowly and invade surrounding structures; consequently, these tumors require surgical removal with a good cure rate. A rarer but more invasive type, thymic carcinoma, is harder to manage and could require surgery, chemotherapy, and/or radiation.
Lymphomas are the second most common mediastinal tumor, and account for one fourth of all anterior mediastinal tumors. The most common types are Hodgkin lymphoma and B-cell lymphoma.
Q: What complications are associated with mediastinal tumors?
A: Complications of mediastinal tumors may include spinal cord compression (numbness, pain, weakness) and the spread of either benign or malignant tumors to nearby structures such as the heart and great vessels (aorta and vena cava).
Q: What are the symptoms of mediastinal tumors?
A: Sixty percent of patients with mediastinal tumors experience symptoms. These include cough, feeling of fullness in the chest, shortness of breath, substernal pain, and weight loss.
Other possible symptoms include fever/chills, night sweats, coughing up blood, swollen lymph nodes, respiratory blockage, and hoarseness.
At Stony Brook University Hospital, we provide leading-edge multidisciplinary care
to give all patients with mediastinal tumors the best possible outcomes.
Q: How are mediastinal tumors diagnosed?
A: A CT scan of the chest is the most commonly used imaging study to define the mediastinal tumor size and extension. Once the tumor mass is confirmed, a biopsy is usually indicated.
A CT-guided needle biopsy is occasionally possible and sufficient to make a diagnosis.
A cervical mediastinoscopy is another diagnostic technique. It consists of a small incision made at the base of the neck. It allows the visualization and biopsy of any growths around the airway (via direct vision or with the help of a miniature camera).
Other diagnostic surgeries include an endobronchial ultrasound-guided biopsy, or a thoracoscopic biopsy (usually excisional).
Q: How are mediastinal tumors treated?
A: Depending on the cause, a mediastinal tumor can be watched (an asymptomatic and non-enlarging cyst). Once a diagnosis is confirmed, the treatment can range from surgical removal (thymic tumors) to chemotherapy (lymphomas or germ cell tumors).
Q: What kind of surgery is used to treat them?
A: Once a decision is made to surgically remove a mediastinal tumor, there generally are two approaches that are used: an anterior approach done through a cut in the front of the chest and breastbone (sternum), called a sternotomy; or a lateral approach done through tiny incisions on the side of the chest, in between ribs, with a minimally invasive procedure called VATS.
VATS stands for video-assisted thoracoscopic surgery. A thoracoscope is a tiny video camera that transmits images of the inside of the chest onto a video monitor, guiding the surgeon in performing the procedure.
VATS might be performed with a surgical robot; that is, a high-tech instrument the surgeon may use to achieve the most precise surgery. Robotically-assisted VATS require not only the technology but special expertise on the part of the surgeon.
Our thoracic surgeons at Stony Brook Medicine use the latest technology,
and they have many years of experience in treating patients with mediastinal tumors.
Q: What are the risks of surgery for mediastinal tumors?
A: As with any surgery, there is always a small risk of bleeding or infection. However, due to the location of the mediastinal tumors, there is an extra layer of surgical complexity due to the proximity of vital structures such as the heart and esophagus that have to be preserved.
Q: What is the survival rate for patients with cancerous mediastinal tumors?
A: Most surgically removed mediastinal tumors have a favorable outcome. The kind of tumor, the stage, and the surgical margins status dictate the ultimate outcome. Non-surgical tumors like lymphomas also respond readily to chemotherapy.
Q: What is the advantage of having mediastinal tumors treated at Stony Brook Medicine?
A: At Stony Brook University Hospital, we provide leading-edge multidisciplinary care to give patients with mediastinal tumors the best possible outcomes. Our surgeons use the latest technology, and have many years of experience in treating patients with these tumors.
Patients can undergo video-assisted thoracoscopic surgery (VATS) for the removal of mediastinal tumors. This approach uses small incisions, and provides faster recovery than traditional procedures that require large incisions and opening the chest.
If the tumor is more extensive or potentially invading vascular structures, a sternotomy (incision in middle of chest) or hemi-sternotomy (incision in upper half of chest) is commonly used.
Rarely, the removal of the tumor requires placing the patient on cardiopulmonary bypass — a procedure used for open heart surgery to temporarily bypass the heart function — to allow for a more aggressive surgery to take out the tumor.
In less sophisticated hospitals without bypass machines, these tumors would be deemed inoperable and, instead of surgery, patients would be treated with chemotherapy or radiation. Such an approach may be less than ideal because surgery has been shown to provide the best outcomes.