
Compassion combined with the latest treatment options define our care, which is delivered by our specialized team of Urologists all trained in urogynecology and female pelvic reconstructive surgery.
The subspecialty of female urology is concerned with the diagnosis and treatment of urinary tract disorders, most prevalent in females (urinary incontinence, overactive bladder, pelvic organ prolapse, recurrent urinary tract infection, and pelvic pain). Expert evaluation of these conditions includes a complete history and physical exam, as well as additional bladder studies such as Urodynamics (i.e. bladder function test), imaging studies (i.e. CT Scan and/or MRI), and cystoscopy. The Department of Urology at Stony Brook offers comprehensive evaluation and treatment for all female urologic disorders.
Our team practices at our
Women's Pelvic Health and Continence Center
located at: 140 N. Belle Mead Road, East Setauket
What is Voiding Dysfunction?
Voiding dysfunction is an umbrella term for urinary problems and can affect individuals in different ways. The main symptoms are urinary frequency, urgency, painful urination and/or incomplete bladder emptying. Treatment is aimed at decreasing or eliminating symptoms and may involve medication or pelvic floor relaxation exercises. Please explore the conditions listed below to learn more.
Common Conditions
Urinary incontinence is the medical term for accidental bladder leakage. This condition is more common in older women and is not a normal part of aging.
Symptoms
Stress Incontinence:
- Leak urine when you laugh, cough, or sneeze
- Common in women who have had a baby
Urgency Incontinence:
- Feeling a strong need to urinate suddenly
- Urge to urinate is so strong that you cannot make it to the bathroom in time
Mixed Incontinence: Having symptoms of both stress and urgency incontinence.
If you are experiencing the above symptoms see a doctor to learn more about the treatment options available
Treatments we offer
- Lifestyle modifications (weight loss, diet, constipation, limit smoking)
- Pelvic floor muscle (Kegel) exercises
- Bladder retraining (following strict scheduled bathroom times)
- Medicines to relax the bladder
- Bladder botox injections
- InterStim ("Bladder pacemaker")
- Percutaneous tibial nerve stimulation
- Surgery (mesh or non-mesh slings)
Helpful Resources on Urinary Incontinence:
Overactive bladder is defined by the sudden, urgent need to urinate. Sudden urination may occur at any time of the day.
Symptoms
- Urinating more than 8 times per day
- The need to urinate at night
- Sudden urges to urinate
- May also be experiencing urinary incontinence (leakage)
If you are experiencing the above symptoms see a doctor to learn more about the treatment options available.
Treatments options
- Lifestyle changes
- Limit fluid intake to 4-6 glasses (8-ounce) of fluid per day
- No fluids after dinner
- Avoid the following:
- Tobacco
- Coffee and Tea
- Carbonated beverages
- Alcohol
- Spicy foods
- Chocolate
- Acidic fruits (oranges, cranberry, pineapple, etc.)
- Losing weight to reduce pressure on the bladder
- Retraining your bladder (following strict scheduled bathroom times)
- InterStim ("Bladder pacemaker")
- Percutaneous tibial nerve stimulation
- Bladder botox injections
- Surgery
Urinary tract infections (UTI) occur when bacteria gets into the urethra (the tube that carries urine from the bladder to the outside). These bacteria infections can occur in either the bladder or kidney. A UTI is considered recurrent when the patient experiences an infection more than 2 times in a 6-month period, or more than 3 times in one year.
Symptoms
| Bladder Infection Symptoms | Kidney Infection Symptoms |
|---|---|
|
|
Visit your doctor if you are experiencing any of the symptoms above to determine a treatment method.
Treatments we offer| Bladder Infection Treatments | Kidney Infection Treatments |
|---|---|
|
|
Interstitial cystitis, also called “bladder pain syndrome,” is a condition that causes people to have bladder pain and need to urinate often. This condition is more common in women, and doctors suspect that it is caused from abnormal changes in the lining of the bladder.
Symptoms
- Bladder pain that gets better after urinating
- Feeling like you need to urinate (even if you do not actually urinate)
Symptoms of interstitial cystitis are different from person to person. Some people might not have symptoms on a daily basis. Some symptoms get worse based on diet, monthly cycles, sitting for a long period of time, or stress.
If you have the symptoms listed above, visit your doctor to get an exam and complete a urine test. Other tests, such as a cystoscopy, may be performed to see if the bladder is abnormal.
Treatments we offer
- Bladder training - holding in urine for longer periods of time
- Physical therapy - to prescribe exercises to relax belly, groin, and buttocks
- Medicine - pill or liquid forms to heal the bladder lining or to reduce pain
- Surgery - a small device is placed in the lower back to connect a nerve that goes to the bladder
Helpful Resources on Interstitial Cystitis:
Many females suffer from sexual dysfunction. As it is an embarrassing situation, they frequently fail to consult a physician for help. There is currently significant research being conducted on female sexual dysfunction.
Symptoms and Causes
A common symptom of this condition is dyspareunia or painful sexual intercourse. This is frequently due to physiological changes related to a decline in female hormones. This leads to a decrease in the secretions normally responsible for vaginal lubrication during sexual intercourse. Other symptoms of female sexual dysfunction include orgasmic difficulties and low sexual desire associated with depression or dyspareunia.
Diseases of the female pelvic organs, such as endometriosis, may affect the blood or nerve supply of the genitalia and be responsible for sexual difficulties in females. In such cases, pelvic surgery may be an option.
How is Female Sexual Dysfunction Evaluated?
A detailed history and physical examination will usually reveal the cause of the problem. In difficult cases of female sexual dysfunction, a pelvic or vaginal ultrasound may provide more definitive answers to this problem. Fortunately, current advances have produced revolutionary pharmacological agents, which are available for females with sexual dysfunction. If you believe you suffer from Female Sexual Dysfunction, do not hesitate to seek help from Stony Brook Urology's specialist in Female Urology.
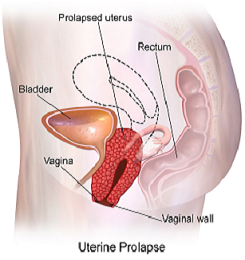
Pelvic Organ Prolapse (POP) is a hernia of the pelvic organs (bladder, uterus, rectum). This type of hernia occurs if the muscles surrounding the organs are weakened. It is most common in women after giving birth, or those going through menopause. There are two types of pelvic organ prolapse:
- Asymptomatic POP - the hernia has occurred, but no tissues protrude beyond the vaginal opening
- Symptomatic POP - the hernia has occurred, and tissues are protruding beyond the vaginal opening
Symptoms
- Vaginal pressure - while standing, coughing, exercise
- Feeling heavy in the pelvic area
- Feeling a bulge in the vaginal opening
If you are experiencing the above symptoms see a doctor to learn more about the treatment options available.
Treatments options
- Pelvic floor muscle strengthening (Kegel exercises)
- Physical therapy - for a customized strengthening plan
- Losing weight
- Vaginal estrogen
- Vaginal pessary (small, removable device that keeps prolapse inside)
Surgical Options
- Cystocele Repair - repairs the bladder or urethra
- Hysterectomy - complete removal of the uterus
- Rectocele Repair - repairs the rectum
- Vaginal vault suspension - laparoscopic surgery to repair the vaginal walls
- Vaginal obliteration - closing of the vagina
Female Reconstructive Surgery
 What is Female Reconstructive Surgery?
What is Female Reconstructive Surgery?
Female Reconstructive Surgery is used to restore the organs of the pelvic floor to their normal position. This is typically performed on women with pelvic floor prolapse caused by damage during childbirth or suffering from urinary incontinence. The surgery used for this condition is a robotic-assisted sacrocolpopexy.
How it Works
At Stony Brook, we utilize the da Vinci Robot to insert a small telescope and make several incisions in the prolapsed organs. With the help of the da Vinci Robot, the surgeon can use specially designed tools to attach a graft of tissue or synthetic mesh onto the pelvic organs. The graft is then attached to a bony area, allowing the organs to be placed back to their normal position.
- Following the procedure patients may experience back pain and constipation for 2-4 weeks
- Gentle walking / swimming is allowed
- Avoid heavy lifting and strenuous exercise
- Patients should avoid sexual intercourse for 6 weeks
- Patients can return to normal activity levels gradually
There is the possibility of complications including mesh erosion or infection if the mesh moves from the vaginal wall into nearby organs.
Physicians
 |
 |
 |
| Jason M. Kim, MD Associate Professor Female Urology Voiding Dysfunction Pelvic Floor Reconstruction |
Steven Weissbart, MD Associate Professor Female Urology Voiding Dysfunction Pelvic Floor Reconstruction |
Justina Tam, MD Assistant Professor Female Urology Voiding Dysfunction Pelvic Floor Reconstruction |
Clinical Staff
 |
 |
 |
| Erin Henkes, NP | Jennie Jacob, MS, PA-C | Yvonne Kwok-Lin, NP |
 |
 |
|
| Olga Makrak-Sturniolo, NP | Stephanie Kramer, MS, PA-C |

